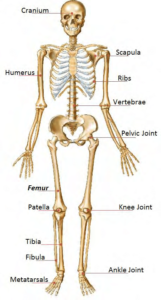
Anatomy of the Bones
 The adult human skeleton has a total of 213 bones, excluding the sesamoid bones. The appendicular skeleton has 126 bones, axial skeleton 74 bones, and auditory ossicles six bones. Each bone constantly undergoes modeling during life to help it adapt to changing biomechanical forces, as well as remodeling to remove old, microdamaged bone and replace it with new, mechanically stronger bone to help preserve bone strength.
The adult human skeleton has a total of 213 bones, excluding the sesamoid bones. The appendicular skeleton has 126 bones, axial skeleton 74 bones, and auditory ossicles six bones. Each bone constantly undergoes modeling during life to help it adapt to changing biomechanical forces, as well as remodeling to remove old, microdamaged bone and replace it with new, mechanically stronger bone to help preserve bone strength.
The four general categories of bones are long bones, short bones, flat bones, and irregular bones. Long bones include the clavicles, humeri, radii, ulnae, metacarpals, femurs, tibiae, fibulae, metatarsals, and phalanges. Short bones include the carpal and tarsal bones, patellae, and sesamoid bones. Flat bones include the skull, mandible, scapulae, sternum, and ribs. Irregular bones include the vertebrae, sacrum, coccyx, and hyoid bone. Flat bones form by membranous bone formation, whereas long bones are formed by a combination of endochondral and membranous bone formation.
The skeleton serves a variety of functions. The bones of the skeleton provide structural support for the rest of the body, permit movement and locomotion by providing levers for the muscles, protect vital internal organs and structures, provide maintenance of mineral homeostasis and acid-base balance, serve as a reservoir of growth factors and cytokines, and provide the environment for hematopoiesis within the marrow spaces.
The long bones are composed of a hollow shaft, or diaphysis; flared, cone-shaped metaphyses below the growth plates; and rounded epiphyses above the growth plates. The diaphysis is composed primarily of dense cortical bone, whereas the metaphysis and epiphysis are composed of trabecular meshwork bone surrounded by a relatively thin shell of dense cortical bone.
The adult human skeleton is composed of 80% cortical bone and 20% trabecular bone overall. Different bones and skeletal sites within bones have different ratios of cortical to trabecular bone. The vertebra is composed of cortical to trabecular bone in a ratio of 25:75. This ratio is 50:50 in the femoral head and 95:5 in the radial diaphysis.
Cortical bone is dense and solid and surrounds the marrow space, whereas trabecular bone is composed of a honeycomb-like network of trabecular plates and rods interspersed in the bone marrow compartment. Both cortical and trabecular bone are composed of osteons.
Cortical osteons are called Haversian systems. Haversian systems are cylindrical in shape, are approximately 400 mm long and 200 mm wide at their base, and form a branching network within the cortical bone. The walls of Haversian systems are formed of concentric lamellae. Cortical bone is typically less metabolically active than trabecular bone, but this depends on the species. There are an estimated 21 × 106 cortical osteons in healthy human adults, with a total Haversian remodeling area of approximately 3.5 m2. Cortical bone porosity is usually <5%, but this depends on the proportion of actively remodeling Haversian systems to inactive cortical osteons. Increased cortical remodeling causes an increase in cortical porosity and decrease in cortical bone mass. Healthy aging adults normally experience thinning of the cortex and increased cortical porosity.
Cortical bone has an outer periosteal surface and inner endosteal surface. Periosteal surface activity is important for appositional growth and fracture repair. Bone formation typically exceeds bone resorption on the periosteal surface, so bones normally increase in diameter with aging. The endosteal surface has a total area of approximately 0.5 m2, with higher remodeling activity than the periosteal surface, likely as a result of greater biomechanical strain or greater cytokine exposure from the adjacent bone marrow compartment. Bone resorption typically exceeds bone formation on the endosteal surface, so the marrow space normally expands with aging.
Trabecular osteons are called packets. Trabecular bone is composed of plates and rods averaging 50 to 400 mm in thickness. Trabecular osteons are semilunar in shape, normally approximately 35 mm thick, and composed of concentric lamellae. It is estimated that there are 14 × 106 trabecular osteons in healthy human adults, with a total trabecular area of approximately 7 m2.
Cortical bone and trabecular bone are normally formed in a lamellar pattern, in which collagen fibrils are laid down in alternating orientations . Lamellar bone is best seen during microscopic examination with polarized light, during which the lamellar pattern is evident as a result of birefringence. The mechanism by which osteoblasts lay down collagen fibrils in a lamellar pattern is not known, but lamellar bone has significant strength as a result of the alternating orientations of collagen fibrils, similar to plywood. The normal lamellar pattern is absent in woven bone, in which the collagen fibrils are laid down in a disorganized manner. Woven bone is weaker than lamellar bone. Woven bone is normally produced during formation of primary bone and may also be seen in high bone turnover states such as osteitis fibrosa cystica, as a result of hyperparathyroidism, and Paget’s disease or during high bone formation during early treatment with fluoride.
The periosteum is a fibrous connective tissue sheath that surrounds the outer cortical surface of bone, except at joints where bone is lined by articular cartilage, which contains blood vessels, nerve fibers, and osteoblasts and osteoclasts. The periosteum is tightly attached to the outer cortical surface of bone by thick collagenous fibers, called Sharpeys’ fibers, which extend into underlying bone tissue. The endosteum is a membranous structure covering the inner surface of cortical bone, trabecular bone, and the blood vessel canals (Volkman’s canals) present in bone. The endosteum is in contact with the bone marrow space, trabecular bone, and blood vessel canals and contains blood vessels, osteoblasts, and osteoclasts.